Claims rejected either by the clearing house or payer end up on the Claim Errors list. Unlike the Prep Errors list, not all of the errors can be fixed within the Encounter or Patient, as some may have nothing to do with data errors, but rather with policy issues, such as cancelled coverage, etc. Therefore, these errors will likely require more research and communication with the insurance companies and patients.
Perform the following steps to Review Claim Errors:
- From the Claims menu on the left side of the screen, select Review Claim Errors.
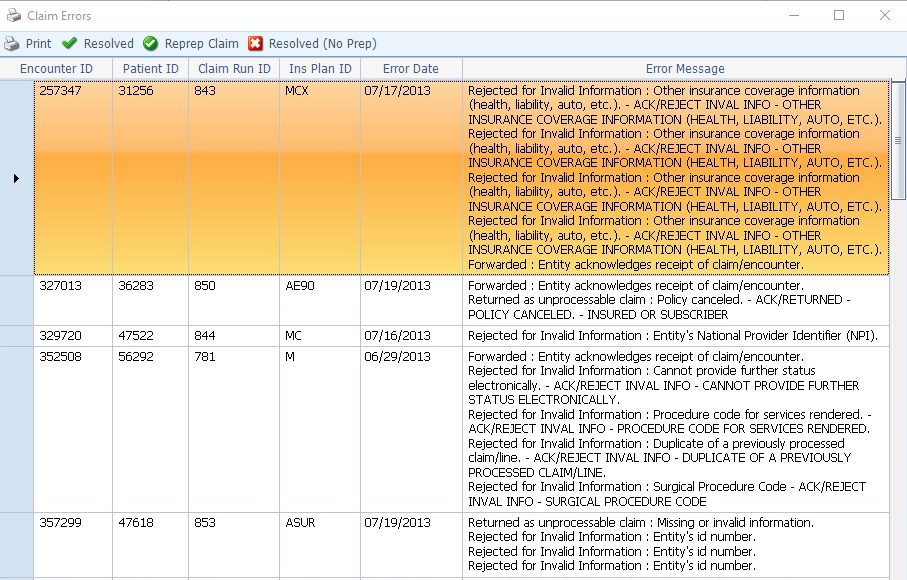
The Claim Errors screen will appear, as shown below.
- Go down the list and fix errors as described in the Error Message Column.
- If the error is Encounter related, click the Encounter number. The Encounter will open in edit mode, allowing you to make corrections, save and close.
- If the error is Patient related, click the Patient number. The Patient record will open in edit mode, allowing you to make corrections, save and close.
- As you fix each error, mark it as corrected (which drops it from the Claim Errors list) in one of two ways:
- Click Resolved on the toolbar. This will open a Notes box to allow you to document the actions you took for future reference. It will check if you have Re-prepped the claim (either from the Claim Errors screen or from the Encounter itself) and prompt you to do so if you have not.
—or—
- Click Resolved (No Prep) if you do not wish to re-submit the claim to the same payer, either because it has become the patient’s responsibility or because it needs to go to a different payer.
- Repeat for each subsequent error on the list.

