Primary Insurance Reimbursement Report
- Referral Report
- Patient Appointment Report
- Claim Adjustment Report (CAR codes)
- General Navigation
- Aging Report
- Apply Credits
- Closing Run Summary
- Collection Payment Summary
- Facility Report
- Insurance Aging Report
- Patient Roster Report
- Primary Insurance Reimbursement Report
- Recall Report
- Service Reimbursement Report
- Service Status Report
- Tickle Note Report
- Transaction Detail Report
- Update Billing Account Types
- Month End
The Primary Insurance Reimbursement Report is used primarily to analyze the practice’s fee structure or for negotiating contracts with various insurance payers. It can also be used to manage payments with current contracted insurance companies.
Filter Selection
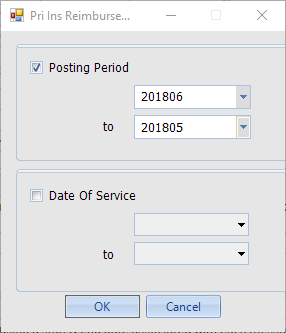
Report can be filtered either by Posting Period or Date of Service range.
The Report

For each CPT posted, the report lists the fee, each insurance plan payment received, and the allowable for comparison and analysis. This is a dynamic report that allows for additional grouping and sorting. Selecting a row and clicking Ledger pulls up the Service line on the Patient Ledger for additional details.

